Physical Therapy: Your Complete Guide to Faster Recovery, Lasting Pain Relief & Peak Mobility
How many mornings have you rolled out of bed, felt a stab of knee or back pain, and wondered, “Will this ever get better?” Whether you’re a desk-bound professional, a weekend athlete, or someone rehabbing a surgery, the answer often lies in physical therapy (PT). Globally, 619 million people already live with low-back pain alone, and projections show that figure climbing toward 843 million by 2050. Yet PT services remain underused, even though the data prove they can shorten recovery, curb future disability, and save thousands of dollars in medical costs.
This guide cuts through jargon and marketing hype. You’ll learn exactly when to seek PT, what to expect in each session, and which evidence-based home exercises keep you moving between appointments. We’ll also dive into 2025’s biggest trends—telehealth, virtual reality, AI-powered wearables—and break down the latest Medicare rules so you’re never blindsided by a bill. Ready? Let’s rebuild your body.
Table of Contents
Physical Therapy 101: Why It Matters Right Now
The scale of the problem
Musculoskeletal (MSK) conditions affect 1.71 billion people worldwide, making them the top driver of disability. When joints stiffen or nerves flare, people move less, gain weight, and spiral into chronic disease. Physical therapists break that cycle by restoring movement earlier, faster, and more safely than medication alone.
Evidence speaks louder than painkillers
Still tempted to wait it out? Early PT for new-onset low-back pain slashes downstream health-care costs by roughly US $4,160 and lowers the likelihood of injections or surgery. Similar savings appear for neck pain, rotator-cuff tears, and knee arthritis.
Direct access = no referral headaches
All 50 U.S. states, D.C., and the Virgin Islands now allow at least an initial evaluation without a physician’s prescription, though some still add time or visit caps. Booking a consult has never been simpler.
Thought-provoking question: What would you regain first—sleep, sports, or mood—if pain dropped by half next month?
Do You Need PT? 10 Quick Self-Checks
If you answer “yes” to any item below, consider scheduling an evaluation.
- Pain or stiffness lasting more than 14 days with no clear improvement.
- Repeated ankle, knee, or shoulder sprains despite “rest and ice.”
- Tingling or numbness, shooting down an arm or leg.
- Post-operative weakness (e.g., ACL reconstruction) beyond the surgeon’s expectations.
- Balance issues or frequent falls.
- Gradual decline in walking endurance or stair capacity.
- Unexplained headaches are linked to neck tension.
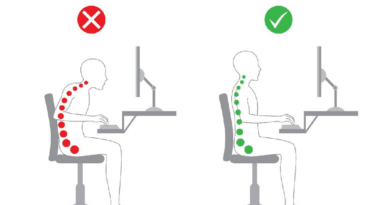
- Poor posture plus workday fatigue—(spoiler: slouching isn’t always the villain).
- A sports or fitness goal that stalled because of nagging discomfort.
- You simply want credible movement advice instead of generic internet workouts.
Treatment Options Explained
Physical therapy is more than “soft-tissue massage and clamshell exercises.” Below are the core categories you’ll encounter:
Manual Therapy
Joint mobilization, soft-tissue release, neural glides. Skilled hands can ease pain, unlock range, and prime muscles for exercise.
Therapeutic Exercise
From motor-control drills for spine stability to blood-flow-restriction (BFR) training after knee surgery, your plan is highly personalized and progresses as you heal.
Modalities
Heat, cold, ultrasound, low-level laser… useful as adjuncts—never stand-alone solutions. Ask your therapist why each modality is chosen.
Tele-Rehabilitation
Meta-analyses show tele-PT delivers equal or better patient-reported outcomes versus traditional care for many MSK issues. Great for rural dwellers and busy professionals.
Virtual & Augmented Reality (VR/AR)
VR-based gaming systems improve upper-limb function after stroke and balance in chronic low-back pain. AR tools such as Stroll lay visual cues that transform Parkinson’s gait.
Wearable Sensors & Mobile Apps
Smart sleeves track knee-bend angles post-replacement, while military-funded programs beam real-time gait coaching to veterans at home. Data replaces guesswork.
Reader prompt: Could a sensor-packed sleeve nudge you to finish that final rep when motivation dips?
The Step-by-Step Roadmap: From First Visit to Graduation
- Pre-visit prep. Jot symptom patterns, surgeries, meds, and personal goals. Upload previous imaging, if any.
- Initial Evaluation (60-75 min). History, movement screens, strength tests, and baseline outcome scores. You’ll leave with a printed or app-based home exercise program (HEP).
- Plan of Care. Typical frequency is 1–3 sessions/week for 4–12 weeks, adjusted using objective metrics (range, force output, walking speed).
- Progress Reviews. Every 2–3 weeks, your therapist retests function and updates goals.
- Graduation & Maintenance. When you meet discharge metrics—e.g., pain < 2/10, symmetry > 90 %—PT shifts to a self-directed fitness plan. Annual “movement physicals” are encouraged to catch relapses early.
Finding the Right Therapist
1. Credentials & Specialties
Look for the DPT (Doctor of Physical Therapy) degree plus board certification—OCS (Orthopedics), SCS (Sports), NCS (Neurologic), or PCS (Pediatrics).
2. Key Questions to Ask
- “What percentage of your caseload matches my condition?”
- “How will we measure progress?”
- “Will I see the same provider each visit?”
3. Red Flags
High-pressure package sales, generic printouts with no form checks, or claims that passive machines “fix everything.” Evidence shows exercise, education, and patient-driven goals are non-negotiable for lasting change.
Home Exercise Programs That Work
Always clear new exercises with your PT, especially post-surgery.
1 Low-Back Pain Starter Set
| Move | Reps × Sets | Why It Helps |
| Cat-Camel | 10 × 2 | Restores segmental mobility without loading discs. |
| Bird Dog | 8 each side × 3 | Trains core-to-hip coordination. |
| Hip Bridge | 12 × 3 | Wakes glutes—often inhibited when pain strikes. |
(Estimated time: 8–10 minutes)
2 Post-ACL Phase 2 Highlights (Weeks 4 – 8)
- Open-chain knee extensions 90–30°
- Heel raises with BFR
- Stationary bike intervals: 10 × 30 seconds, moderate pace
3 Desk-Job Posture Circuit
- Thoracic extension over chair back × 30 seconds
- Band pull-aparts × 15
- Stand-up micro-break: 2-minute brisk walk every 30 minutes—shown to outshine pricey ergonomic chairs.
Reflection moment: Which of these moves could you weave into a lunch break today?
Lifestyle Levers That Boost PT Results
1 Sleep
Aim for 7–9 hours. Poor sleep amplifies pain sensitivity and impairs collagen repair.
2 Nutrition
Protein (1.2–1.6 g/kg), omega-3s, and colorful produce fight inflammation; adequate vitamin D supports bone healing.
3 Physical Activity Minimums
Government guidelines urge 150 minutes of moderate aerobic + 2 strength days weekly. Your PT can convert those targets into joint-friendly routines.
4 Stress & Mental Health
Mindfulness and graded exposure lower the fear-avoidant behaviors that stall progress.
Cost, Insurance & Telehealth in 2025
- Medicare Part B covers PT after the annual deductible; 2025 therapy thresholds (“KX modifiers”) adjust each January.
- The 2024 Physician Fee Schedule saw a 2.93 % hike mid-year.
- Pandemic-era telehealth flexibilities now run through September 30, 2025, letting you join sessions from home without rural-site restrictions.
- Typical U.S. cash rates range US $75–$150 per visit; bundled packages may drop the per-session cost, but read the fine print.
- Cost-saving strategies:
- Use direct access to start treatment sooner (fewer visits later).
- Combine in-person and tele-PT for hybrid efficiency.
- Master your HEP to reduce dependency.
- Use direct access to start treatment sooner (fewer visits later).
Frequently Asked Questions
Q 1: Will insurance refuse to pay if I self-refer?
Most plans honor direct-access visits, but some require a physician’s signature after a set number of sessions. Verify with customer service before visit #1.
Q 2: Is soreness after PT normal?
Mild muscle soreness (24-48 h) is expected; sharp joint pain isn’t. Flag intense or lingering discomfort to your therapist.
Q 3: How soon after surgery should PT begin?
For many procedures—ACL, rotator-cuff repair, spine fusion—rehab starts within 1–5 days to protect tissue and prevent stiffness. Follow surgeon/PT joint protocols.
Q 4: Can virtual reality replace “real” therapy?
VR is a tool, not a replacement. Data shows it augments motivation and neural retraining, especially in neuro and chronic-pain cases.
Q 5: Why does my PT keep asking about sleep or stress?
Healing is systemic. Cortisol, blood sugar, and mood all influence tissue repair and pain perception.
Final Takeaway
Physical therapy in 2025 blends hands-on expertise with cutting-edge tech to restore movement, slash pain, and future-proof your body. The sooner you start, the less you’ll spend—and the faster you’ll reclaim the activities that make life yours. So what’s keeping you from booking that first session? Your future self is already thanking you.
References
- Vos T, et al. Lancet study on global low-back pain prevalence, 2020. PMC
- WHO Fact Sheet: Low-Back Pain, 2023. World Health Organization (WHO)
- WHO Fact Sheet: Musculoskeletal Conditions, 2023. World Health Organization (WHO)
- APTA Direct Access Advocacy page, 2024. American Physical Therapy Association
- APTA “Choose PT” cost-savings analysis for acute LBP, 2023. choosept.com
- VA/DoD Stroke Rehabilitation Guideline, 2024. VA.gov | Veterans Affairs
- OHSU ACL Reconstruction Protocol, Feb 2024. OHSU
- PubMed Systematic Review—Tele-Rehabilitation Effectiveness, 2023. PubMed
- CMS Therapy Services updates (KX thresholds), Jan 2025. CMS
- CMS CY 2024 Physician Fee Schedule Update, Mar 2024. CMS
- Medicare Telehealth Extension (H.R. 1968), Mar 2025. Kiplinger
- PubMed RCT—VR Stroke Upper-Extremity Rehab, 2024. PubMed
- JMIR Protocol—VR for Chronic LBP, 2024. JMIR
- Sensors Article—Wearable Tech in Knee Rehab, 2025. PMC
- DHA News—Mobile Device Outcomes-Based Rehab, Apr 2025. dha.mil
- Time magazine analysis on posture myths, 2024. Time
- The Times back-pain relief article, 2024. Latest news & breaking headlines
- JAMA Network Open—Lifestyle Care vs Guideline Care for LBP, 2025. JAMA Network
- Physical Activity Guidelines for Americans, 2nd ed. (ODPHP), 2024. Ohio Department of Health
- CDC Physical Activity Basics page, 2024. CDC